Benefits of a Chronic Care Management Program
Data-proven improvements in patient outcomes
Patient outreach services drive patient retention and loyalty
CMS strongly supports new CCM service models and reimbursements
CCM drives increase in meaningful, reimbursable, in-office E&M encounters
- Increase in Medicare Shared Savings Program attributable beneficiaries
- Improves accuracy of patient risk scoring, impacting capitulated reimbursements models
CCM improves MIPS and APM quality measure scoring

Earn Recurring Revenue
DocIndy provides all of the benefits of Chronic Care Management, with none of the hassles. With reimbursement rates ranging from approximately $40 to $142, Medicare’s Chronic Care Management bill code 99490, 99487, and 99489 afford practices the opportunity to create a new profit center while improving the experience and clinical outcomes for patients.
-
No upfront money
-
No software or hardware to purchase
-
No new staff to hire
-
Contingency pricing
We don't get paid, until you get paid.
Turn Key CCM
24/7 Patient Access

Patient and Provider Portals
Custom Patient Care Plans
Secure File Sharing
Simplified CCM Billing for Providers
How does it work?
We provide the services, you collect from Medicare, we charge a percentage of what you collect.
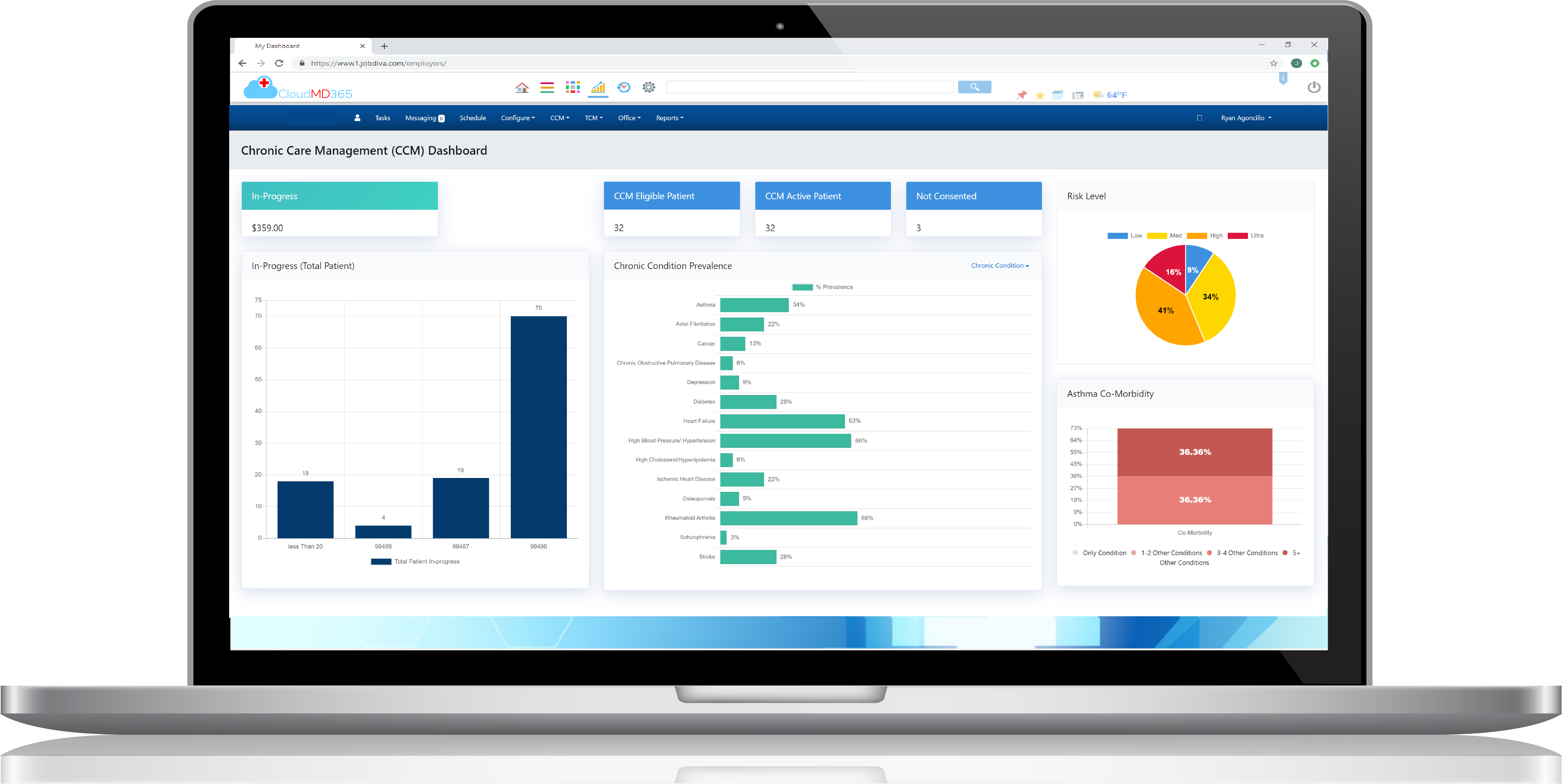
CCM Software Designed with clinicians in mind.
Find out why practices everywhere are choosing DocIndy to simplify their Chronic Care Management program:
-
Your own secure, HIPAA-compliant software portal
-
Unlimited users and patients
-
Live Dashboard showing current CCM minutes
-
Patent-pending Guided-interviews for CCM Care Plans
-
Task tracker (with timer) and Time Logging
-
Monthly Update interface for clinical staff and providers
-
Create Care Plan reports for patient and other providers
-
Easily download summaries and upload to your EHR
-
Integrates with Annual Wellness Visit Software
-
Easy Billing interface to easily submit 99490 claims
-
Tech Support via email and phone

READY TO GET STARTED?
Find out how much you could save using our CCM Cost Calculator.